June Pearl #3: Vasopressin for upper GI bleed.
Pearl: If vasopressors are needed as a bridge to definitive therapy, vasopressin should be the first used because patients with cirrhosis have a relative deficiency in vasopressin. - John Schneider MD PGY4
This was a pearl I heard up in the MICU during my rotation there as we would often receive these patients as transfers or from our own ED who were awaiting for an endoscopy for banding or other therapy. In addition to ceftriaxone, IV PPIs, blood products, and octreotide if a vasopressor was needed I was taught to start vasopressin with the theory that cirrhosis patients have a relative deficiency in vasopressin. In fact, we would start it at 0.08 U/min. I had never investigated the evidence behind this pearl until recently. Below is a discussion on some of the evidence.
Vasopressin deficiency?
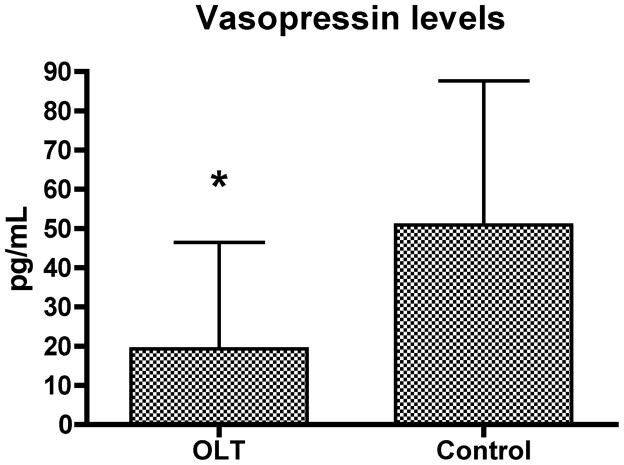
Source: adapted from Wagener et al. (cited below)
This is likely based off a 2010 study that compared vasopressin levels in the pre-operative setting in liver transplant patients with liver disease compared to similar procedures with a normal functioning liver. This was a very small study (28 patients), but did show a statistically significant difference in the level of vasopressin between the two groups (figure on right). They also demonstrated an improvement in MAP and SVR with the administration of vasopressin. While the evidence is not part of a large body of work, it is reasonable to conclude that our variceal bleeding patients might be vasopressin deficient. The question then remains, is there evidence that vasopressin is the correct first vasopressor for these patients?
The Evidence
Some of the prominent studies on vasopressin are outlined in on Life in the Fast Lane’s information sheet on vasopressin found here. These studies are for septic shock, which is also believed to cause a relative deficiency in vasopressin.
The three major studies I looked into are summarized below:
VAAST Trial: NEJM 2008: This was a double blind, multicenter study that randomized patients on low dose norepinephrine to either more norepinephrine or vasopressin. While there was no significant difference in mortality at 28 days among all patients there was a trend towards improvement in mortality at both 28 days and 90 days in lower severity patients with vasopressin. Of note, this paper led to the recommendation for use as an adjunctive pressor agent (at a lower 0.03 U/min dose) int he 2008 update to the surviving sepsis guidelines.
VANISH Trial: JAMA 2016: This was a double blind, factorial (2x2) multicenter randomized study that compared norepinephrine to vasopressin in patients with or without hydrocortisone. The main outcome of this study was numbers of days alive and free of kidney failure (stage 3 defined by AKIN). There was no difference between the two drugs.
Nagendran et al, ICM 2009: This was an individual data meta analysis that compared vasopressin with other vasoactive agents. There was no effect on 28 day mortality. One important finding from this study is that vasopressin was shown to have an increase in digital ischemia.
My Take Away
Upper GI bleed patients with liver failure may indeed have a deficiency in vasopressin. Most of the studies with vasopressin are in septic shock patients, but given infection is believed to be part of the underlying pathology in variceal bleeds there is probably some application of this data to patients with variceal bleeds. This data shows neither a significant advantage nor disadvantage compared to norepinephrine as a bridge to definitive therapy in patients in extremis from an upper GI bleed.
Vasopressin considerations
Pros:
effects are preserved during hypoxia and severe acidosis and catecholamine-resistent states
less pulmonary artery vasoconstriction than norepinephrine
less arrhythmia than norepinephrine
Cons:
can cause digital ischemia and
should not be used without a central line (see first point) as there is no antidote
can cause unintented coronary vasoconstriction
Other FOAM
Maryland Critical Care Project Lecture: on Acute Upper GI Bleeds: http://maryland.ccproject.com/2013/07/29/critical-pearls-for-acute-upper-gi-bleed/
EM RAP Critical Care Mailbag June 2020 (login required): https://www.emrap.org/episode/emrap2020june/criticalcare
Emcrit IBCC Vasopressors chapter:
https://emcrit.org/ibcc/pressors/#pure_vasopressors
Life in the fast lane: Vasopressin
https://litfl.com/vasopressin/
Other Primary Literature
Clinical use of vasopressin in the management of bleeding esophageal varices: https://pubmed.ncbi.nlm.nih.gov/6983321/#:~:text=Vasopressin%20has%20been%20used%20for,venous%20blood%20flow%20and%20pressure.
Vasopressin in liver disease — should we turn on or off?
Citations:
Wagener G, Kovalevskaya G, Minhaz M, Mattis F, Emond JF, Landry DW. Vasopressin deficiency and vasodilatory state in end-stage liver disease. J CardiothoracVascAnesth. 2011;25(4):665–670.
Russell JA, Walley KR, Singer J, Gordon AC, Hébert PC, Cooper DJ, Holmes CL, Mehta S, Granton JT, Storms MM, Cook DJ, Presneill JJ, Ayers D; VASST Investigators. Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med. 2008 Feb 28;358(9):877-87
Nagendran M, Russell JA, Walley KR, et al. Vasopressin in septic shock: an individual patient data meta-analysis of randomised controlled trials. Intensive Care Med. 2019
Blog Post Author and Pearl Provider: John E. Schneider MD PGY4